Abstract
Introduction: FLT3-ITD occurred in about 25% of adult patients with acute myeloid leukemia (AML), which has been correlated with poor outcomes mainly in cytogenetically normal AML, thus being one of the most frequently affected genes in AML. Whether allogeneic hematopoietic stem cell transplantation (allo-HSCT) can eliminate the detrimental effects of FLT3-ITD mutation in AML patients remain debatable. Studies from our group and others showed that allo-HSCT may overcome the adverse effect of FLT3-ITD on survival outcomes, comparable outcomes were not confirmed in other studies. Additionally, high allelic ratio was correlated with inferior outcomes while NPM1 mutation was associated with favorable outcomes in several studies, but their association with prognosis was not observed in other studies. Previous study from our group showed comparable outcomes between FLT3-ITDmut and FLT3-ITDwt patients, however, the influence of NPM1 mutation and allelic ratio on FLT3-ITDmut patients remains unclear in our database. Hence, we designed a retrospective matched-pair study to compare the survival outcomes between FLT3-ITDmut and FLT3-ITDwt patients who underwent allo-HSCT and further analyzed the impact of NPM1 and allelic ratio on outcomes.
Methods: 118 FLT3-ITDmut patients and 497 FLT3-ITDwt patients undergoing allo-HSCT were observed. Each FLT3-ITDmut patients was matched with three FLT3-ITDwt patients using the nearest neighbor-matching method with a caliper size of 0.2. Age and sex of patients, disease status, cytogenetics, pre-MRD, and follow-up days were included in the propensity score model.
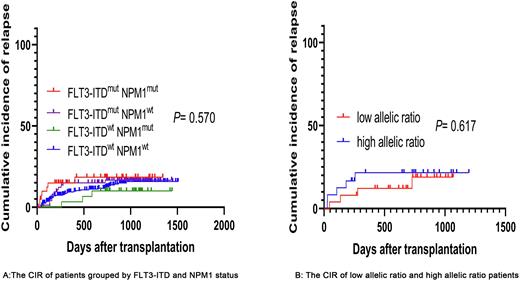
Results: 116 FLT3-ITDmut patients and 314 FLT3-ITDwt patients were included with a median (range) age of 35 years (1-64). FLT3-ITDmut patients showed higher WBC counts at diagnosis (P<0.001) and NPM1 mutation rate (P<0.001). CIR and LFS of FLT3-ITDmut patients were similar to FLT3-ITDwt patients (CIR:16.9% vs 14.2%, P= 0.266; LFS: 75.1% vs 77.7%, P= 0.399). 32 patients and 41 patients showed NPM1 mutation in FLT3-ITDmut and FLT3-ITDwt patients, respectively. We divided them into four groups based on the status of FLT3-ITD and NPM1 status, no significant difference in CIR and LFS was observed between FLT3-ITDwt NPM1wt, FLT3-ITDwt NPM1mut, FLT3-ITDmut NPM1wt and FLT3-ITDmut NPM1mut patients (FLT3-ITDwt NPM1wt vs FLT3-ITDwt NPM1mut vs FLT3-ITDmut NPM1wt vs FLT3-ITDmut NPM1mut: CIR: 14.8% vs 9.4% vs 16.4% vs 17.8%, P= 0.570; LFS: 76.9% vs 84.4% vs 79.5% vs 67.1%, P= 0.176). 49 patients with available allelic ratio were divided into low allelic ratio (n=25) and high allelic ratio groups (n=24) according to a cut-off 0.50. High allelic ratio was not correlated with inferior outcomes in this study (high allelic ratio vs low allelic ratio: CIR: 21.1% vs 18.1%, P= 0.617; LFS: 70.6% vs 73.7%, P= 0.563). To further analyze the differences between different donor type, we compared the outcomes of 318 haploidentical transplantation and 98 sibling-matched transplantation patients, respectively. FLT3-ITDmut patients had higher CIR and lower LFS than FLT3-ITDwt patients among sibling-matched transplantation (CIR:24.7% vs 12.0%, P= 0.064; LFS:68.2% vs 83.5%, P= 0.0502), but no difference was observed in haploidentical transplantation (CIR: 13.7% vs 15.0%, P= 0.996; LFS:77.8% vs 75.9%, P= 0.885). FLT3-ITD mutation didn't become a prognostic factor in survival outcomes when all patients received transplantation. Prognostic factors with P< 0.1 in univariate analysis were included in multivariate analysis. Apart from pre-MRD, and disease status influencing OS and CIR, another factor affecting OS was the gender of patients. Age played a prognostic role in NRM while pre-MRD and disease status also became the significant factors influencing LFS.
Conclusion: Our results showed that allo-HSCT, especially haploidentical HSCT, may overcome the adverse effect of FLT3-ITD mutation, regardless of the NPM1 status or allelic ratio. Allo-HSCT could be an ideal option for AML patients with FLT3-ITD.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal